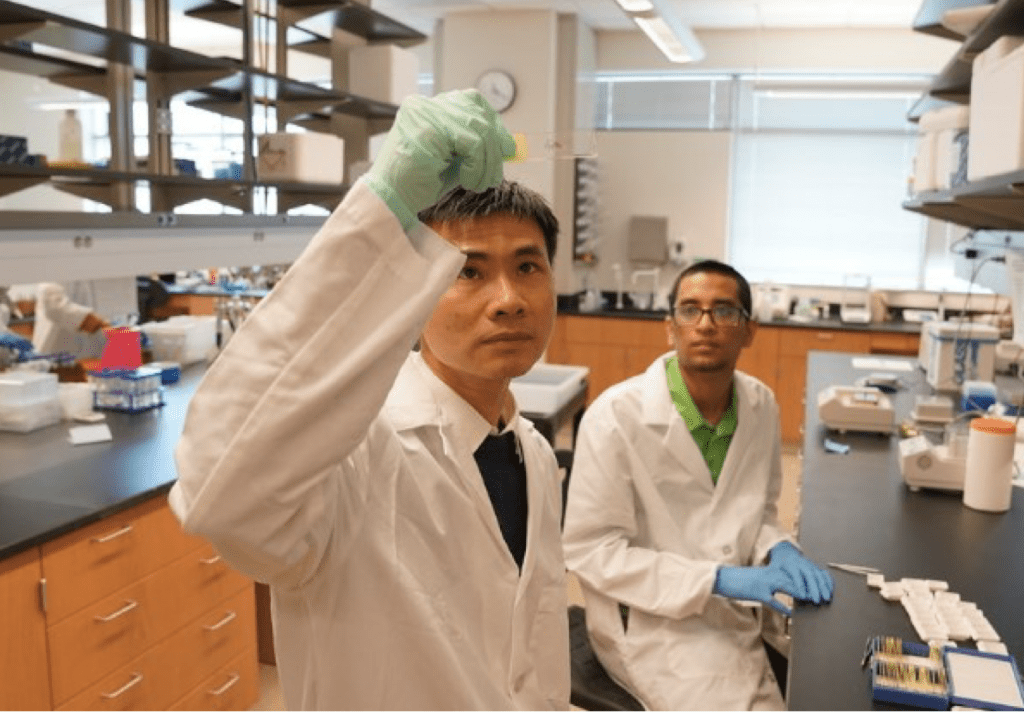
As the Covid-19 virus continues to pose a health threat, scientists are learning how and why the virus affects individuals differently. UCF researcher Dr. Hung Nguyen and his immunology team at the Burnett School of Biomedical Sciences have been studying how metabolic changes in the body affect immune response, with the goal of better predicting who is more susceptible to severe cases of the virus.
The effects of COVID-19 on individuals with metabolic comorbidities like Type 2 diabetes, obesity, and hypercholesterolemia are well known. But the underlying cell mechanisms of why this happens remain unclear. Dr. Nguyen and his team recently published a study in Communication Biology that examined how metabolic cellular changes affect the body’s adaptive immune response to SARS-CoV-2 infections.
The team evaluated blood from hospitalized COVID-19-infected patients to get a systematic understanding of how the virus affects immune cell metabolism. They also did a single-genomics analysis of lymphocytes from the lungs to assess immunity at the direct site of viral infection.
Dr. Nguyen examined natural killer T cells (NKT) and CD8 T cells, which navigate your body’s immune response. He found a significant difference in the metabolism and antiviral efficacy of key immune cell types among COVID patients with severe lung damage that kept their lungs from adequately supplying oxygen to the body. Many of these patients also had pre-existing metabolic comorbidities.
To survive and thrive, immune cells convert oxygen, food and sugar into energy. Dr. Nguyen’s group found that in response to decreased oxygen and altered nutrient availability from COVID, immune cells were forced to shift to other oxygen-independent pathways to generate energy. In addition, they compensated by eating their own mitochondria – a biological process known as mitophagy. “As immune cells continue to fight in these metabolically challenged conditions, they become exhausted and have impaired anti-viral function,” he explained.
Thanks to the body’s immunological memory cells, people who have already been infected with a virus usually mount a faster immune response to re-infection. UCF researchers found, however, that metabolically challenged conditions kept the immune system from creating memory cells, making these patients more vulnerable to COVID reinfection.
“We were able to identify crucial metabolic biomarkers that could be applied to predict COVID-19 severity,” said Dr. Nguyen.
Using high-dimensional flow cytometry, advanced metabolomics and bioinformatics technology, UCF undergraduate student Sanjeev Gurshaney, who collaborated on the paper, conducted a comprehensive analysis of metabolic processes in differing types of immune cells.
“Now we can show that during severe COVID-19, the availability of oxygen and other key nutrients, along with the ways in which cells process them to generate energy, are critical in determining their anti-viral function,” Gurshaney said, who was recently honored with UCF’s Order of Pegasus, the university’s highest student recognition.
They also found that administering a drug which blocks mitophagy allowed the previously weakened immune cells to recover their ability, proliferate memory cells and regularize their metabolism.
“By being able to identify novel biomarkers that can predict the severity of the virus in patients, it will be possible to develop better therapies for severe COVID-because we have a more comprehensive picture of immune cell metabolism and function,” said Dr. Nguyen.
UCF collaborators on the paper include AdventHealth Research Institute, Houston Methodist Research Institute, La Jolla Institute for Immunology, and MD Anderson Cancer Center.