Biography
Background
Research in the Rohde Lab: Research in the Rohde lab is focused on pathogenic mycobacteria, including the slow-growing Mycobacterium tuberculosis (Mtb), which causes >10 million new infections and ~1.5 million deaths each year, and M. abscessus (Mab), a rapidly growing non-tuberculous mycobacteria (NTM) that afflicts people suffering from pre-existing conditions such as cystic fibrosis (CF) and chronic obstructive pulmonary disorder (COPD). Current treatment options for both Mtb and Mab are inadequate, requiring 4-12 months of multidrug regimens that fail to achieve a durable cure in many cases. This problem is exacerbated by the increasing incidence of antibiotic resistant Mtb and Mab. Development of novel antibiotics to treat these pulmonary infections is hindered by many knowledge gaps regarding mechanisms of virulence and drug resistance. There is also a need for improved, affordable diagnostics to detect mycobacterial infections that require treatment at the point-of-care (POC). To help address these problems, my group is pursuing a multi-faceted approach that encompasses 1) discovery and development of new antibiotic candidates able to eradicate drug resistant Mtb/Mab, 2), design and preclinical evaluation of a novel POC diagnostic platform for Mtb/NTM, 3) development of innovative genetic tools (CRISPRi) and establishment of a CF-mouse model for assessing drug targets in Mab, and 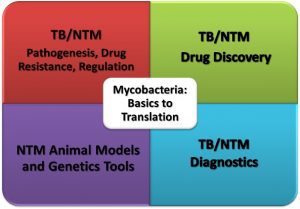 4) molecular microbiology studies of Mtb/Mab pathogenesis, gene regulation, and mechanisms of drug resistance. We have been continuously funded by NIH and the Cystis Fibrosis Foundation for the past 10+ years to support these endeavors. Strategic collaborations with diverse scientists including synthetic/medicinal/natural product chemists, structural biologists, and biochemists have made these diverse, exciting adventures in science possible.
4) molecular microbiology studies of Mtb/Mab pathogenesis, gene regulation, and mechanisms of drug resistance. We have been continuously funded by NIH and the Cystis Fibrosis Foundation for the past 10+ years to support these endeavors. Strategic collaborations with diverse scientists including synthetic/medicinal/natural product chemists, structural biologists, and biochemists have made these diverse, exciting adventures in science possible.
Research Areas
1) TB/NTM Drug Discovery. The establishment of a BSL3 screening facility for drug screening against Mtb at UCF and the development of a robust pipeline of assays has positioned the Rohde lab as one of a relatively small number of labs nationwide with these capabilities. This has enabled multiple parallel drug discovery projects in partnership with different synthetic/medicinal chemistry collaborators. Implementation of a Mtb-mouse infection model in the Lake Nona ABSL3 further enhances our value as a partner in drug discovery. The “hits” that we discover through these efforts represent valuable candidates for hit-to-lead development and chemical biology tools we can exploit to discover new drug targets.
-
A) Next-gen β-lactams targeting mycobacteria. Until recently, the β-lactam class of antibiotics has been overlooked as a useful therapeutic for TB/NTM infections because of the lack of efficacy of penicillin and other clinically used β-lactams. New insights into the unique targets of β-lactams in mycobacteria, development of β-lactamase inhibitors to overcome the major resistance mechanisms, and the discovery of β-lactamase-resistant carbapenems (a subclass of β-lactams) effective against mycobacteria has reinvigorated interest in this area of research. This collaborative project hinges on the pioneering synthetic chemistry efforts of Dr. John Buynak (SMU) who has devised schemes to generate “next-gen” carbapenems with unprecedented atypical modifications that confer enhanced activity against mycobacteria and improved pharmacological properties. This project, initially supported by an NIH R15 award to Dr. Buynak on which I was a co-Investigator, was recently awarded a ~$3.5 million R01 grant enabling addition of a biochemist (Dr. Basta, US Naval Academy) and structural biologist (Dr. Korotkov, U. Kentucky) to the team. Thus far, we have discovered atypical carbapanems with enhanced potency against Mtb and Mab, resistance to β-lactamase inactivation, ability to overcome natural resistance mechanisms in Mab clinical isolates, and improved pharmacokinetic properties.
-
B) Resistance-proof halogenated phenazines (HPs) with a novel mechanism of action. In an R21 funded project in collaboration with Dr. Rob Huigens III (UF), we are building on our discovery of a class of natural-product inspired synthetic compounds we call HPs with potent antimicrobial activity against both MRSA biofilms and mycobacteria. Top compounds are very potent against multiple mycobacteria species, highly selective (low mammalian toxicity), and active against dormant drug-tolerant bacilli. They appear to act via a unique mechanism of action (MoA) involving intrabacterial metal chelation and generation of reactive oxygen species, rather than binding and inhibition of an essential enzyme. This is consistent with our inability to detect the emergence of resistant mutants in Mtb, a desirable trait for a new antibiotic. Initial characterization of anti-mycobacterial HPs was published in J. Med. Chem (IF=8.04) in 2021. Our work continues to develop even more potent lead compounds for in vivo testing and more fully elucidate their mechanism of action.
- C) Novel gyrase inhibitors targeting Mtb. Fluoroquinolones (i.e. moxifloxacin, gatifloxacin) are second-line anti-TB agents clinically used for treatment of multi-drug resistant TB (MDR-TB), however they are associated with side effects and toxicity problems. They function through inhibition of DNA gyrase, an enzyme critical for chromosome replication. Finding novel gyrase inhibitors that lack these downsides offers a promising strategy for developing new TB drugs. In a project recently funded by an NIH R21 award, in collaboration with Dr. Fenfei Leng (FIU, biochemist and gyrase expert) and Dr. Adel Nefzi (FIU, synthetic chemist), we will develop and characterize multiple novel, non-fluoroquinolone gyrase inhibitors active against Mtb that were discovered in a high-throughput screen devised by Dr. Leng.
Development of additional TB/NTM early-stage drug candidates is underway including a marine natural product derived inhibitor of dormant Mtb, inhibitors of novel targets involved in mycomembrane synthesis, protein translation, and metabolism, and characterization of hits from AI-driven virtual screens of 30+ million compounds.
2) TB/NTM Diagnostics. This area of research is an extension of a very productive collaboration with Drs. Dmitry Kolpashchikov and Yulia Gerasimova (UCF, Dept. of Chemistry). We are exploiting deoxyribozyme (Dz) sensor technology to develop point-of-care diagnostic assays for detection of Mtb and NTM, detection of mutations that confer drug-resistance in Mtb, and for speciation of NTM which is crucial for determination of appropriate therapy. We have developed assays with both fluorescent and visual readouts, and tested designs that combine Dz sensors with multiplex PCR or isothermal amplification products. Under our NIH R01 funded project for which I am lead MPI (co-MPI Dr. Gerasimova, UCF; Dr. da Silva, FURG/Brazil; co-I Dr. Brian Kim UCF), we have developed a prototype fluorescent assay for detection and species identification of Mtb and 5 most clinically relevant NTMs. Despite some significant setbacks due to COVID, we have implemented this assay in Dr. da Silva’s lab in Brazil and completed preclinical evaluation on a large panel of clinical isolates. Work is underway to complete the fabrication of a 3D-printed fluorescent real-time PCR device to complete the proposed POC assay prototype.
3) NTM Animal Model and Genetic Tools. In addition to the lack of significant investment in NTM research (until recently), the lack of suitable animal models for chronic NTM infections and lack of validated genetic tools for opportunistic mycobacteria like Mab have hampered progress in this field. Supported by awards from Cystic Fibrosis Foundation and NIH, we have sought to address these needs and apply new tools to study drug resistance mechanisms (CFF) and drug targets (NIH) in Mab. To attempt to develop a mouse model for Mab pulmonary infection, we have established a breeding colony of transgenic b-ENAC mice which mimic the mucus-laden airway phenotype of CF patients via overexpression of an ion channel in pulmonary epithelial cells. Secondly, we have implemented CRISPRi technology in Mab, validating a tool for inducible silencing of target genes. We are applying CRISPRi to i) assess the function of predicted drug resistance genes, and ii) to quantitatively evaluate the vulnerability of essential genes to inhibition/silencing as a means to prioritize putative drug targets. Combining CRISPRi and the b-ENAC mouse model, our goal is to evaluate the “druggability” of targets within the complex pulmonary environment that imposes unique stresses on the pathogen that can alter metabolism and growth.
4) NTM Pathogenesis and Gene Regulation. Two-component systems (TCS) and Mab stress responses. As recently published by my lab, we have characterized a species-specific regulon controlled by the DosRS TCS required for adaptation of Mab to hypoxia. Although the Mtb DosRS ortholog is arguably the best characterized mycobacterial TCS, we noted a surprising lack of overlap in the complement of genes controlled by DosRS in each species. Thus, elucidating the novel role of DosRSMab and other TCSs will require in-depth studies and extrapolating from Mtb studies may be of limited utility.
Rohde Lab Publications:
-
Neves YCd, Reis AJ, Rodrigues MA, Chimara E, da Silva Lourenço MC, Fountain J, Ramis IB, von Groll A, Gerasimova Y, Rohde KH, Almeida da Silva PE. 2024. Detection of Mtb and NTM: preclinical validation of a new asymmetric PCR-binary deoxyribozyme sensor assay. Microbiol Spectr. Jun 4;12(6):e0350623. doi: 10.1128/spectrum.03506-23. Epub 2024 Apr 23. PMC11237447.
-
Simcox BS, Rohde KH. 2024. Orphan response regulator NnaR is critical for nitrate and nitrite assimilation in Mycobacterium abscessus. Front Cell Infect Microbiol. May 24;14:1411333. doi: 10.3389/fcimb.2024.1411333. eCollection 2024. PMC11162112.
-
Atomwise AIMS Program (Geden S., Rohde KH et al.). 2024. AI is a viable alternative to high throughput screening: a 318-target study. Sci Rep. Apr 2;14(1):7526. doi: 10.1038/s41598-024-54655-z. PMC10987645.
-
Simcox B, Tomlinson BR, Shaw LN, Rohde KH*. 2023. Mycobacterium abscessus DosRS two-component system controls a species-specific regulon required for adaptation to hypoxia. Frontiers Cell Inf Microbiol. Mar 9:13:1144210. PMC10034137.
- Gupta R, Rohde KH*. 2023. Implementation of a mycobacterial CRISPRi platform in Mycobacterium abscessus and demonstration of the essentiality of ftsZMab. Tuberculosis (Edinb). Jan:138:102292.
- Miranda-Velez M, Sarker GS, Ramisetty P, Geden S, Bartolomeu Halicki PC, Annamalai T, Tse-Dinh YC, Rohde KH, Moon JH. 2022. Proton Motive Force-Disrupting Antimycobacterial Guanylurea Polymer. Nov 14:23(11):4668-4677.
- Si A, Landgraf AD, Geden S, Sucheck SJ*, Rohde KH*. 2022. Synthesis and Evaluation of Marine Natural Product-Inspired Meroterpenoids with Selective Activity toward Dormant Mycobacterium tuberculosis. ACS Omega. June 27;7(27):234847-23496. *co-corresponding authors
- Gupta R, Al-Kharji N, Alqurafi M, Nguyen T, Chai W, Quan P, Malhotra R, Mortimer P, Simcox B, Brammer-Basta L*, Rohde KH*, Buynak J.* 2021. Atypically modified carbapenem antibiotics display improved anti-mycobacterial activity in the absence of b-lactamase inhibitors. ACS Infect Dis. Aug 13; 7(8):2425-2436. *co-corresponding authors
- Yang Ho, Kundra S, Chojnacki M, Liu K, Fuse M, Abouelhassan Y, Kallifidas D, Zhang P, Huang G, Jin S, Ding Y, Luesch H, Rohde KH, Dunman P, Lemos J, Huigens III R. 2021. A modular synthetic route involving N-aryl-2-nitrosoaniline intermediates leads to a new series of 3-substitutued halogenated phenazine antibacterial agents. J Med Chem. Jun 10; 64(11):7275-7295 (selected as featured article).
- Rohde KH, Sorci L., 2021. The Prospective Synergy of Antitubercular Drugs with NAD Biosynthesis Inhibitors. Front Microbiol. Jan 26: 11:634640.
- Dhar BC, Reed AJ, Mitra S, Rodriguez Sanchez P, Nedorezova DD, Connelly RP, Rohde KH, Gerasimova YV. 2020. Cascade of deoxyribozymes for the colorimetric analysis of drug resistance in Mycobacterium tuberculosis. Biosens Bioelectron. Oct 1; 164:112385.
- Ma Z, Abendroth J, Buchko GW, Rohde KH, Davidson VL. 2020. Crystal structure of a hemerythrin-like protein from Mycobacterium kansasii and homology model of the orthologous Rv2633c protein of tuberculosis. Biochem J. Jan 31: 477(2):567-581.
- Rodrigues Felix C, Roberts JC, Winder PL, Gupta R, Diaz MC, Pomponi SA, Wright AE, Rohde KH*. 2019. Plakinamine P, A steroidal alkaloid with bactericidal activity against Mycobacterium tuberculosis. Mar Drugs. Dec 16:17(12).
- Schneider A, Wood HN, Geden S, Greene CJ, Yates RM, Masternak MM, Rohde KH*. 2019. Growth hormone-mediated reprogramming of macrophage transcriptome and effector functions. Sci Rep. Dec 18:9(1):19348.
- Osterman AL, Rodionova I, Li X, Sergienko E, Ma CT, Catanzaro A, Pettigrove ME, Reed RW, Gupta R, Rohde KH, Korotkov KV, Sorci L. 2019. Novel Antimycobacterial Compounds Suppress NAD Biogenesis by Targeting a Unique Pocket of NaMN Adenylyltransferase. ACS Chem Biol. May 17; 14(6):949-958.
- Bengtson HN, Venken T, Willems H, Jacobs A, Reis AJ, da Silva PEA, Homolka S, Niemann S, Hooyberghs J, and Rohde KH*. 2019. Molecular drug susceptibility testing and strain typing by DNA Hybridization. PLoS ONE. Feb 7;14(2):e0212064.
- Bengtson HN, Sidders AE, Gerasimova Y, and Rohde KH*. 2019. Species Typing of Nontuberculous Mycobacteria by use of Deoxyribozyme Sensors. Clin Chem. Feb;65(2):333-341.
- Demers DH, Knestrick MA, Fleeman R, Tawfik R, Azhari A, Souza A, Vesely B, Netherton M, Gupta R, Colon BL, Rice CA, Rodríguez-Pérez MA, Rohde KH, Kyle DE, Shaw LN, Baker BJ. 2018. Exploitation of mangrove endophytic fungi for infectious disease drug discovery. Marine Drugs. Oct 10:16(10).
- Gupta R#, Rodrigues Felix C#, Akerman MP, Akerman KJ, Slabber CA, Wang W, Adams J, Shaw LN, Tse-Dinh YC, Munro OQ, Rohde KH*. 2018. Evidence for Inhibition of Topoisomerase 1A by Gold(III) Macrocycles and Chelates Targeting Mycobacterium tuberculosis and Mycobacterium abscessus. Antimicrob Agents Chemother. Apr 26:62(5). #equal contribution.
- Ma Z, Strickland KT, Cherne MD, Sehanobish E, Rohde KH, Self WT, Davidson VL. 2018. The Rv2633c protein of Mycobacterium tuberculosis is a non-heme di-iron catalase with a possible role in defenses against oxidative stress. J Biol Chem. Feb 2; 293(5):1590-1595.
- Gupta R, Netherton M, Byrd TF, Rohde KH*. 2017. Reporter-based assays for high-throughput drug screening against Mycobacterium abscessus. Frontiers in Microbiology. Nov 10:8:2204.
- Rodrigues Felix C, Gupta R, Geden S, Roberts J, Winder P, Pomponi S, Diaz M, Reed J, Wright A, and Rohde KH*. 2017. Selective Killing Of Dormant Mycobacterium tuberculosis By Marine Natural Products. Antimicrob Agents Chemotherapy. August vol. 61 no. 8 e00743-17.
- Cumming B, Rahman A, Lamprecht D, Rohde KH, Saini V, Adamson J, Russell DG, Steyn AJC. 2017. Mycobacterium tuberculosis arrests host cycle at the G1/S transition to establish long term infection.PLoS Pathogens. 13(5): e1006389. https://doi.org/10.1371/ journal.ppat.1006389.
- Bengtson HN, Homolka S, Niemann S, Reis AJ, da Silva PEA, Gerasimova YV, Kolpashchikov DM, Rohde KH*. 2017. Multiplex detection of extensively drug resistant tuberculosis using binary deoxyribozyme sensors. Biosensors and Bioelectronics. Mar 1;94:176-183. doi: 10.1016/j.bios.2017.02.051.
- Wright AF, Killday KB, Chakrabarti D, Guzmán EA, Harmody D, McCarthy PJ, Pitts T, Pomponi SA, Reed JK, Roberts BF, Rodrigues Felix C, Rohde KH*. 2017. Dragmacidin G, a Bioactive Bis-Indole Alkaloid from a Deep-Water Sponge of the Genus Spongosorites. Mar. Drugs, 15, 16.
- Vanderven BC, Huang L, Rohde KH, Russell DG. 2016. The Minimal Unit of Infection: Mycobacterium tuberculosis in the Macrophage. Microbiology Spectrum, Dec 4 (6).
- Cox AJ, Bengtson HN, Rohde KH, Kolpashchikov DM. 2016. DNA nanotechnology for nucleic acid analysis: Multifunctional molecular DNA machine for RNA detection. ChemComm. 52 (99): 14318-14321.
- Cox AJ, Bengtson HN, Gerasimova YV, Rohde KH, Kolpashchikov DM. 2016. DNA Antenna Tile-Associated Deoxyribozyme Sensor with Improved Sensitivity. Chembiochem. 17 (21); 2038-2041.
- Rohde KH, Michaels HA, Nefzi A, 2016. Synthesis and Antitubercular Activity of 1,2,4-Trisubstituted Piperazines. Bioorganic and Medicinal Chemistry Letters. 26(9):2206-9
- Sandhaus S, Annamalai T, Welmaker G, Houghten RA, Paz C, Garcia PK, Andres A, Narula G, Rodrigues Felix C, Geden S, Netherton M, Gupta R, Rohde KH, Giulianotti MA, Tse-Dinh YC. 2016. Small molecule inhibitors targeting topoisomerase 1 as novel antituberculosis agents. Antimicrob Agents Chemother.. July vol. 60 no. 7 4028-4036.
- Liu Y, Tan S, Huang L, Abramovitch R, Rohde KH, Zimmerman M, Chen C, Dartois V, VanderVen B, and Russell DG. 2016. Immune activation of the host cell induces drug tolerance in Mycobacterium tuberculosis both in vitro and in vivo. J Exp Med. 213(5):809-25.
- Stout MB, Swindell WR, Zhi X, Rohde KH, List EO, Berryman DE, Kopchick JJ, Gesing A, Fang Y, and Masternak MM. 2015. Transcriptome profiling reveals divergent expression shifts in brown and white adipose tissue from long-lived GHRKO mice. Oncotarget. 6(29): 26702-15.
- Gerasimova YV, Cornett EM, Edwards E, Su X, Rohde KH, Kolpashchikov D.M. 2013. Deoxyribozyme Cascade for Visual Detection of Bacterial RNA. Chembiochem. Nov 4;14(16):2087-90.
No information specified.
In The News
-
Nine Faculty Awarded Promotion, Tenure
-
Drs. Almagro-Moreno, Rohde Win Research Incentive Award
-
WMC Action News | Breakthrough bacteria research improves cystic fibrosis
-
Tackling TB: How Florida Scientists Are Working Toward a New Treatment
-
Dr. Rohde Receives Grant To Fight Infection Common in CF Patients
-
Dr. Rohde Featured on The Scientists’ Channel
-
Burnett Undergrad Wins Founder’s Day Award For Tuberculosis Research
-
Ivanhoe: Undersea Life Treats TB: Medicine’s Next Big Thing?
-
WINK: Undersea Life Treats TB: Medicine’s Next Big Thing?
-
WMFE: Deep Sea Sponges Might Hold The Answer To Curing Drug Resistant TB
-
Founders’ Day Honors Outstanding Faculty, Students
-
Biomed Student Receives Prestigious Goldwater Scholarship
-
Dr. Rohde Wins Top UCF Research Award
-
Atlantic Ocean Could Hold Key To Fighting Tuberculosis
-
Burnett Tuberculosis Research Featured On CBS This Morning